Experiencing depression that feels like a heavy weight, covered by a dark cloud
Ursula a 25-year-old high school math teacher described this “heavy thing in my gut and chest, that’s always there. I’ve had it ever since I can remember. I can’t have any fun. If I try to rest or have fun, I get scared that I will lose my focus and end up wasting time and having an aimless life. That’s what my dad drummed into me and I can’t get any peace or joy.”
Experiencing depression for Ursula was a defense against an insecure, possessive mother and a cold, critical, judgmental father; both of whom denied her the chance to find her agency, authenticity, and passions in live.
Experiencing Depression – a sense of defeat arising from self-loathing and masochism
“I’m scared I won’t be able to make and keep a good relationship with a guy. I get too possessive like my mom, and drive guys away. Then I feel so bad, and start working out, dieting and try to be attractive, but it doesn’t really work. I keep trying to be perfect like my dad wanted, but even if I manage it doesn’t last.”
Part of experiencing depression for Ursula was to be masochistic. Causing herself pain by dieting and working out revealed her sense of self-loathing. She was angry because her attempts at perfectionism failed. She didn’t want to be an angry bitter person like her dad. So she cut herself off from that anger. It was better to be numb and not care about anything than to feel the power of anger, as she might become destructive towards others. The fear of turning into a mean aggressive person made Ursula disown her emotions as she turned into a robot. She became self-destructive instead.
Experiencing Depression – paralyzed by a conflict about her self-identity
The emptiness of her robotic life made her listless, ready to give up. Occasionally she felt twinges of envy watching her colleagues enjoy romantic relationships that freed them from trying to be perfect.
Ursula was in a bind. If she stayed on the path of perfection she was destined to be alone and unhappy, envious, and resentful. If she chose the road leading to connection and fun, she wouldn’t be much of anything, and would risk losing any prospective partner to someone more alluring. Using alcohol and weed deadened the worst pain of the heavy weight and hopelessness, but it interefered with her perfectionism so she self-medicated on a variable schedule.
The conflict was unbearable, and impossible to live with. This internal conflict weighed Ursula down, and wrapped her up in the dark cloud. It kept her mummified – preventing her from having to make the choice that would free her of the unhealthy connections to her possessive mother, and cold judgmental father – in other words, she would have to give up her identity and create a healthier one that honored her vitality, talents and endearing qualities leading to a stable, reliable, nurturing romantic relationships. Living in the depression was her only way of staying connected to her parents – shedding them would leave her orphaned psychologically, and no pills, light treatments, mind altering substances, change of diet or brain magnetic stimulation would do the trick. She would need to be reparented in psychotherapy to develop in the way she was deprived of in her childhood.
Experiencing Depression – chemical and neurological understanding dehumanizes the person
Experiencing depression is uniquely personal, even though it is categorized as a mood disorder. There are a set of symptoms that typify this mood disorder, but the lived experience of depression is absent in that description. Referring to the experience of depression as a set of neurological and chemical changes is an attempt at understanding it, but in effect dehumanizes the person, compounding the negative emotional state.
No one knows whether mood changes set off the corresponding physiological shifts, or vice versa. Obviously they influence each other but cannot and shouldn’t overshadow the actual conscious day to day, debilitating and often shameful moment to moment experience of depression.
Yet, all the current research spurred on by ever greater sophisticated technology, has focused on genetic, neurological, chemical, diet related, and bacteriological factors in order to understand the state of depression. The ‘person’ who is experiencing depression has all but been written out of the story.
Experiencing Depression – the relational trauma and unbearable emotions that cause a shutdown
Experiencing depression is often about feeling numb, exhausted, unmotivated, and withdrawn. It’s also about guilt, shame, and existential fears related to a lack of self-worth. Experiencing depression can be a way of shutting down from overwhelming emotions threatening one’s stability, built up over time in unsettled family life. Reducing all these experiences to mere symptoms and chemical changes is debasing and demeaning. Ignoring the lived experience of depression denies the factors that led to it. For some the source are adversities early in life resulting in a long term depression, (Persistent Depressive Disorder). For others depression is sudden and severe, set off by a specific catastrophic psychological event.
Despite the advances in medicine and medical diagnostics, understanding depression has excluded the relational trauma that is a significant precursor to depression. Therefore the treatments that are forged on healing relationships are sidelined. This includes the emotional care that comes from attachment bonds, the faith, patience, and love that is shown to someone who is depressed vital for recovery – much more so, than drugs, light therapy, transcranial stimulation, or other meditative self-care tools.
Experiencing Depression – separating descriptions from causes
A report in Psychopathology, 2024 goes so far as to say that all the descriptions of depression that are used for diagnostic purposes (symptoms relating to sleep, appetite, daily functioning, and elements of emotional deadening are perfunctory – they don’t illuminate causative factors, and as a consequence deflect from finding treatments related to causes.
How then does someone with depression short or long term get to be accurately diagnosed and treated? The lived experience of depression is the primary feature that aids in the discovery of stressors and or overwhelming emotions the person needs to withdraw from, but is totally ignored in this attempt to understand depression.
Experiencing Depression – brain sections and brain waves versus the lived experience of depression
A recent article in Cyborg and Bionic Systems, 2024 found that there was enhanced Theta brainwave activity in the amygdala (the primal emotional – fight, flight, freeze center of the brain) linked to depressive states in rats. How can this finding relate to Ursula’s experience of depression, where she is emotionally squashed, and her perfectionist personality feeds her a diet of defeat? Are theta waves in her amygdala permanently altered, or do they change when she is angry, or lonely, or weighted down? The relationship between experiencing depression on a constant basis and evoking a false depressive state in rats is hardly useful.
Another article focused on brain networks that altered decision making behaviors in areas within the limbic system (primary basic emotional area) when beta oscillations shifted. The researchers, reported in Nature Communications, 2024, that artificially stimulated beta waves in monkeys produced positive and negative behaviors. They went onto suggest that certain oscillations can be linked to depressive states and poor judgement, while others can be linked to more optimistic emotional states and be linked with better judgement.
The authors of the study make an assumption that monkey depressive like behaviors can be extrapolated to humans simply by inducing so called depressive states of inactivity and loss of appetite to someone like Ursula – who is crippled by an undeveloped emotional intelligence, insecure attachment and perfectionism that makes her live on the edge of failure, shame, and anger at her upbringing! Just imagine Ursula having her beta oscillations fiddled with! Is that going to make her more secure and help her find a stable relationship, lifting the heavy weight inside her? No but therapy focused on her family of origin can, because that is where her conflicts lie.
Experiencing Depression – genetic Inheritance versus the lived experience of depression
Experiencing depression may in part be a feature of genetic inheritance. In 2017 the journal Nature Genetics found that DNA analysis combined with personality data uncovered 116 gene variations linked to neuroticism. Genes associated with neuroticism had some overlap with genes linked to a susceptibility to depression and some other psychiatric conditions.
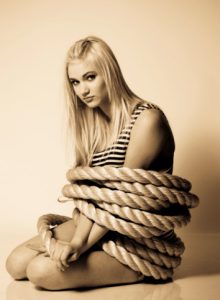
Ursula’s parents may well have been prone to neurotic features. Certainly the possessiveness she felt from her mother, would likely have come from insecure attachment that often leads to the neurotic features of anxiety and depression. Ursula’s soulless, controlling father appears to have had the neuroticism typical of perfectionists who have a constant fear of failure, and no peace of mind – which Ursula certainly inherited. But that doesn’t illuminate Ursula’s experience of depression as an enveloping trapping cloud that lies heavy inside her. The genetic inheritance of neuroticism may make Ursula more prone to bouts of depression, but her experience of being parented by people who couldn’t give her permission to be joyful and at peace probably has the larger effect. Ursula often felt chained to her past unable to develop herself separately from her parents. Trapped in her early childhood relational experiences, which may be expressed in her biology but in no way illuminates experiencng depression from her perspective.
Experiencing Depression – diet and gut microbiome versus the lived experience of depression
Experiencing depression often involves changes in appetite and eating regimen. Some people seek refuge in comfort eating, while others are put off eating – a sort of death-wish, common in some forms of depression. Yet, an article in the May 2024 issue of Nutritional Neuroscience indicates that a poor quality diet per se can reduce the neurotransmitter GABA, reduce gray brain matter, inducing a state of depression. Ursula being a perfectionist robot avoids ultra-processed foods, and dutifully eats the magic Mediterranean diet. She gets no pleasure or energy from it. But her inner voice tells her she is being a good girl. The fact that it brings little reward no matter how well she sticks to the regimen, is even more depressing! So this research doesn’t attend to her lived experience of depression.
Experiencing Depression – memory facilities and cognitive functioning
A report in JAMA Network, 2024, indicates that depressive symptoms can precede memory decline and impair cognitive functioning. In other words, if you are depressed your executive functioning, thinking, planning, decision making and evaluative skills are hindered. The authors also say that poor memory can make someone depressed – emphasizing a bi-directional approach.
Ursula doesn’t want to remember her early traumas where she was used to fill the hole in her mother’s life, when her cold father lived in his own world, being emotionally unavailable to his wife. She didn’t want to stoke the rage that it would evoke inside her, and chose not to remember. Experiencing depression for Ursula was a shield against her rage coming out and possibly turning her life upside down. It’s long been recognized that ‘depression is anger turned inward.’ To keep her ties with her parents, however dysfunctional, meant that Ursula had to keep her intense emotions in check, which meant selective forgetting. At times when she was having a burst of fear that she’d never find a partner, the anxiety would interfere with her cognitive functioning, as it does for us all when we are in fear mode, underpinned by a sense of helplessness and hopelessness.
It’s the purpose of memory loss and the potential survival value that matters, not whether it causes, or is caused by depression.
Experiencing Depression – brain area connectivity versus the lack of motivation, sense of defeat and hopelessness
A 2024 study reported in Molecular Psychiatry suggests that SSRI’s (Serotonin reuptake inhibitors – the most common form of treatment for major depression) and SNRI’s (norepinephrine re-uptake inhibitors) work by restoring connectivity between brain regions, promoting neuro-plasticity. The implication is that there is an imbalance of these neurochemicals, and that by managing the balance, various brain regions reconnect and work in harmony, lifting depression.
Ursula has taken both of these classes of drugs and found unpleasant side effects. She put on weight, and lost her sex-drive – compounding her fear of not being able to attract a partner. If she missed a day of taking the drugs she went into withdrawal – dizziness, nausea, and inability to focus. Whatever connectivity the neurotransmitters enhanced; Ursula’s fear of failure remained. The dark cloud didn’t lift, and that heavy weight inside her gut maintained her emotional paralysis. Her sense of self-worth didn’t change. Her desperation to be perfect accelerated leading to more crashes and hopelessness.
Experiencing Depression – tailoring treatments for various sub-types, versus the lived experience of depression
An important study reported in a 2024 issue of Nature Medicine is one of the only research papers that recognizes that treatments for depression are not a one-size-fits- all panacea. Researchers probed six brain circuits likely associated with depression: the default circuit, attention circuit, salience circuit, negative affect circuit, positive affect circuit, and the cognitive control circuit. Depressed patients who had increased at-rest levels of activity in three regions associated with depression responded best to behavioral therapy.
These people who had overactive cognitive regions of the brain had higher levels of anhedonia (lack of pleasure) and performed worse on executive function (evaluation, planning, judgement, anticipating consequences), but did well on cognitive tasks like thinking through a meal plan.
Those depressed individuals who had low levels of activity (think withdrawn, lethargic, lack of energy, low motivation, poor self-care) did less well with behavioral therapies.
The study attempted to describe the connectivity between brain areas with higher or lower activity and match it with a treatment outcome. The authors in this study did not look at the subjective experience of the depressed people in their samples. Saying that those with high or low activity in various brain areas have similar personal experience of depression is minimizing the unique histories and features of each individual, debasing, and devaluing their personhood.
Experiencing depression as a teen was different for Ursula than her in her early adulthood when she was career focused and living on her own. Her lived experience of depression shifted from one type to another depending on whether her anger was directed at herself for not being a worth a damn (negative self-evaluation) or whether anger was directed at her efforts to be perfect (negative evaluation about her process). Each swing of the pendulum resulted in experiencing depression differently.
Experiencing Depression – Persistent Depressive Disorder requires a psychodynamic approach
Experiencing depression for Ursula within this subtyping, would put her in the category where three parts of her brain regions affecting emotional regulation were key. Talk therapy would suit her best, but what type? The authors probably refer to Cognitive Behavioral Therapy (CBT) as that is the most common talk therapy recommended for a variety of mood disorders. It may deal with certain symptoms that pop up with depression such as with eating, sleeping, and using catastrophic thoughts to keep stuck. However, for someone like Ursula who has Persistent Depressive Disorder characterized by low self-esteem and hopelessness, built on trauma from inadequate and damaging parenting, CBT isn’t going to reparent and facilitate repair and redevelopment.
She needs a more psychodynamic approach where she can feel safe to explore her deep conflicts intertwined with her identity. Yes, Ketamine infusions may open up blocked channels, but it is the psychotherapy that enables the brain areas to connect in ways that establish safety, and permission to be her authentic self.
Copyright, Jeanette Raymond, Ph.D. 2024
You may also like:
Signs of Depression – Origins and Purpose
Fear of Discovering Your True Self Leads to Obsessive Behaviors
How to Save Yourself From your Self-destructive anger. Masochistic Anger Part 1